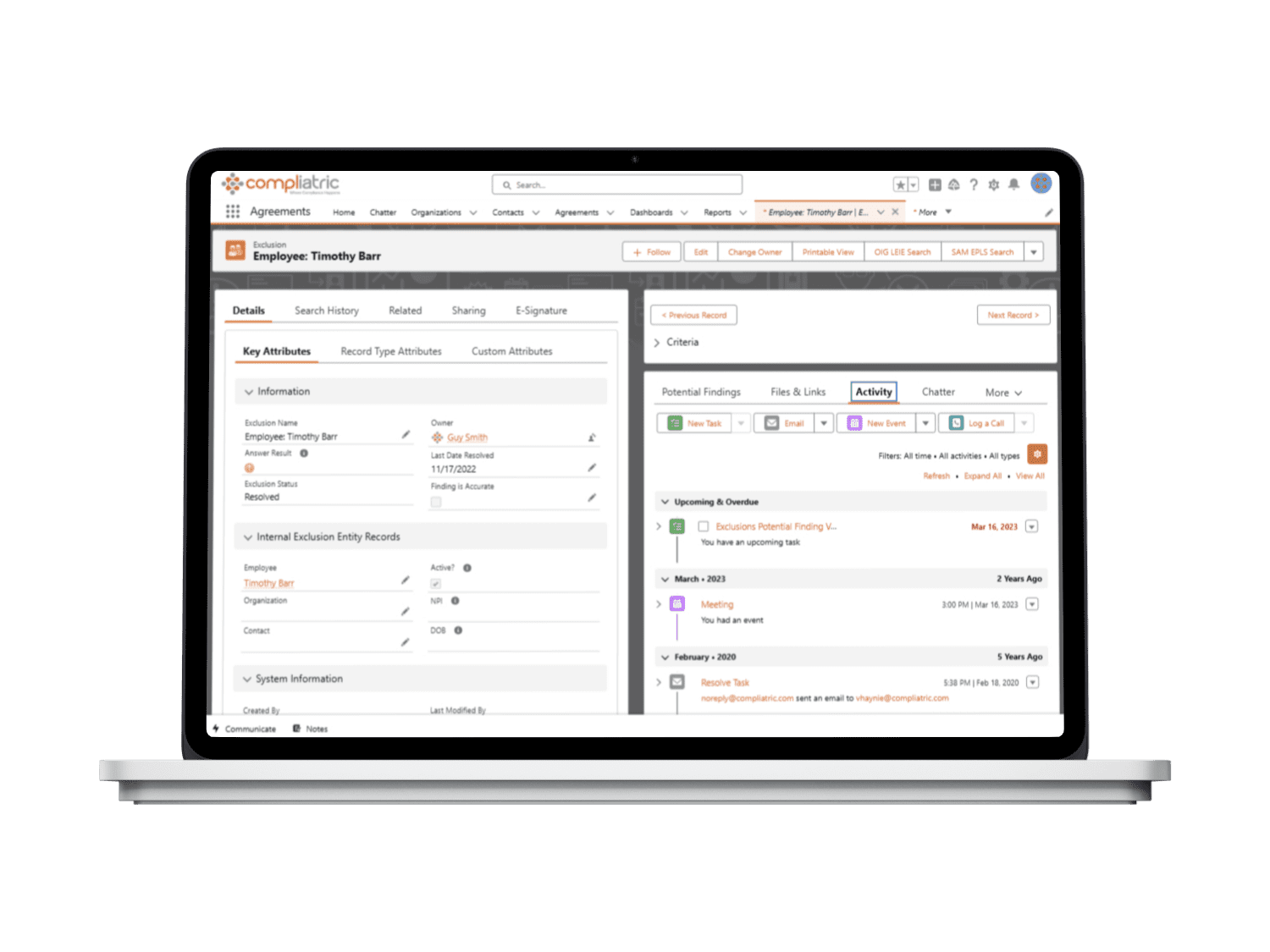
“If I had to use a spreadsheet to manage a new investigation, I could spend a whole day just notating the initial information. Then I’d spend about ten days in the course of a month copying and formatting the rest of the data into a document and attaching all of my supporting information. I can do all of that in an hour with Compliatric.”